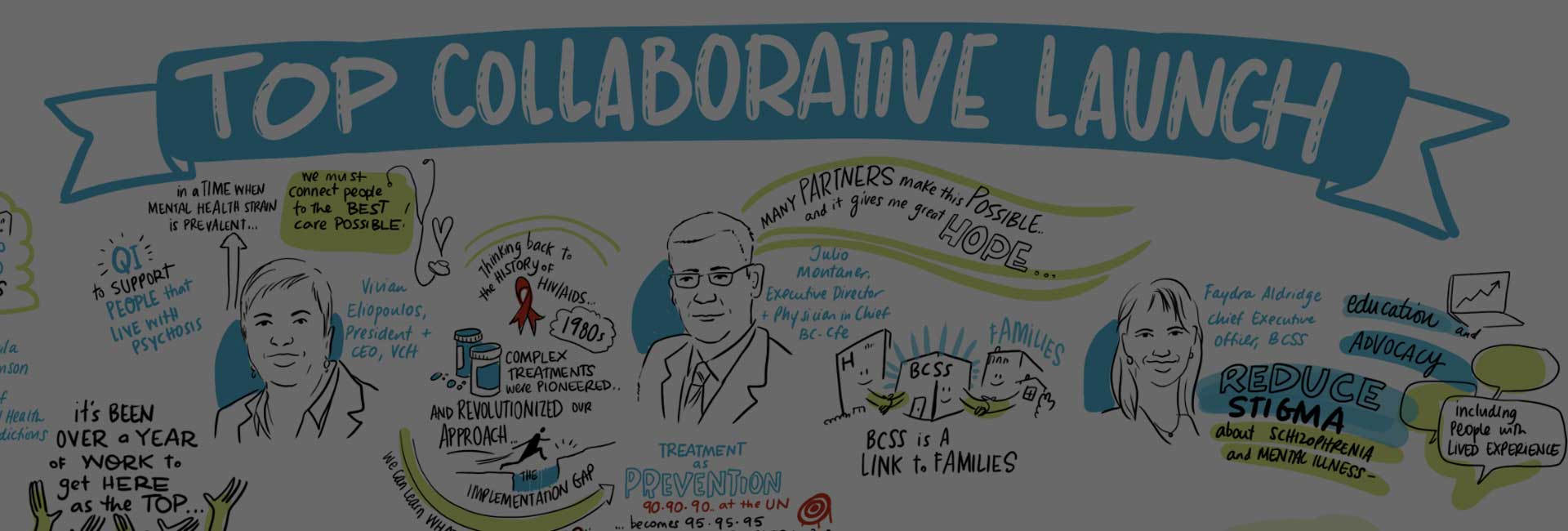
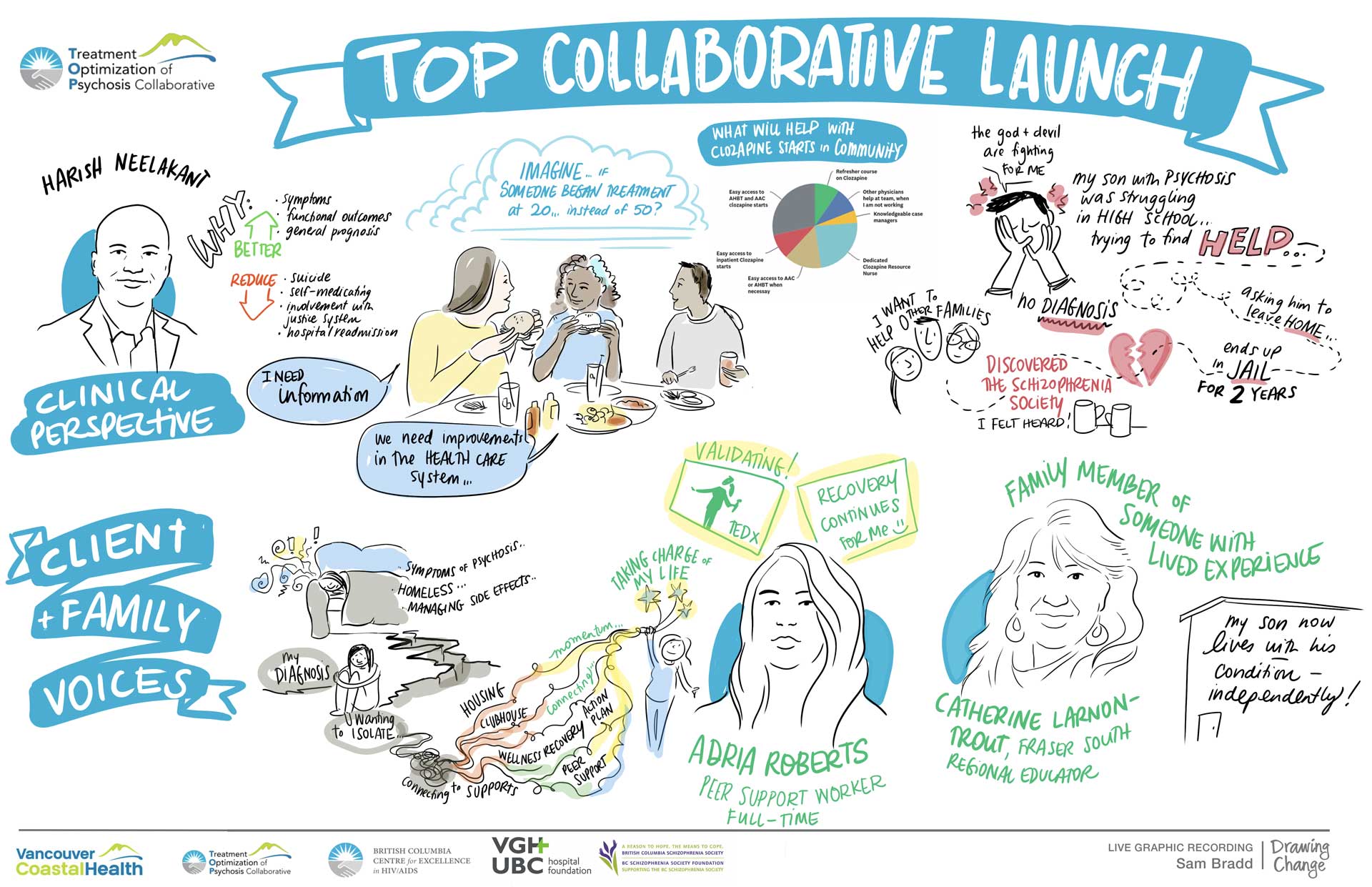
The TOP Collaborative is a quality improvement (QI) initiative led by the BC Centre for Excellence in HIV/AIDS (BC-CfE) in partnership with Vancouver Coastal Health (VCH) Mental Health Services.
Rooted in the experiences and accomplishments of the Treatment as Prevention Strategy (TasP), the BC-CfE has demonstrated capacity for quality improvement (QI) and created a legacy of health system improvement in BC through programs such as the Seek and Treat for Optimal Prevention (STOP) HIV/AIDS Program and the BOOST Collaborative.
Through strong partnerships with VCH in delivering these programs, clients in Vancouver and beyond, have experienced positive change both in the care delivery they receive and in their health outcomes.
The TOP Collaborative will follow the same approach utilizing the Institute for Healthcare Improvement Breakthrough Series Collaborative methodology to support the implementation of the Treatment Optimization of Psychosis (TOP) by shifting initiation from hospital to community settings and by building capacity at each participating community mental health team in the Vancouver Coastal region.
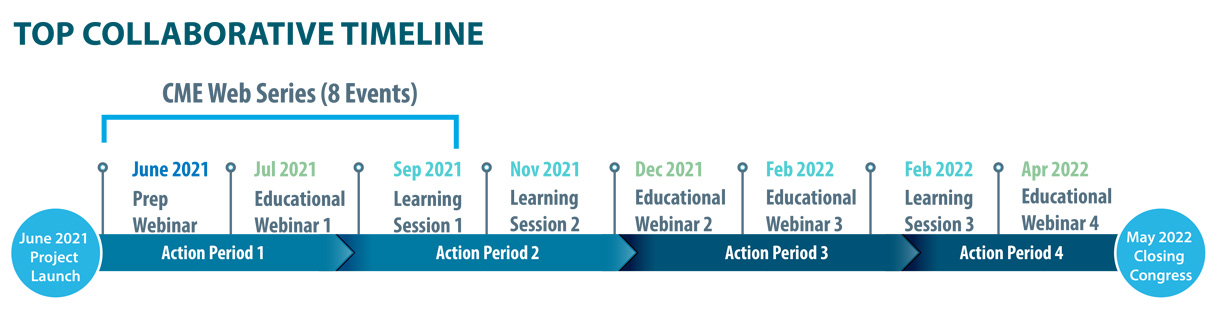
The approach is organized by a series of milestone events and deliverables (see timeline) with monthly reporting on metrics (both quantitative and qualitative). Measurement reporting will be reviewed and analyzed by the Project Team and Collaborative Faculty. Learnings from changes developed during the collaborative will be spread and expanded from participating team members to their colleagues at each site.